L’apnée obstructive du sommeil reste massivement sous-diagnostiquée, en raison d’un accès limité à la polysomnographie. Ici, la prédiction du niveau d’apnée des sujets est réalisée par intelligence artificielle sur la base de la géométrie 3D maxillo-faciale. Tous les participants ont subi une nuit de test de sommeil à domicile ou en laboratoire, et d’autre part une numérisation 3D de leur visage et de leur buste. Les scans 3D craniofaciaux sont traités par morphométrie géométrique, puis par 13 algorithmes d’intelligence artificielle. La combinaison morphométrie géométrique / intelligence artificielle s’avère être une solution rapide et efficace, qui fournit un outil de dépistage peu coûteux pour le syndrome d’apnée du sommeil.
Abstract:
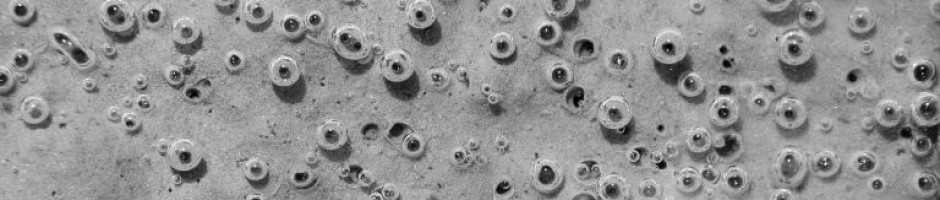
Background: Obstructive sleep apnea (OSA) remains massively underdiagnosed, due to limited access to polysomnography (PSG), the highly complex gold standard for diagnosis. Performance scores in predicting OSA are evaluated for machine learning (ML) analysis applied to 3D maxillofacial shapes. Methods: The 3D maxillofacial shapes were scanned on 280 Caucasian men with suspected OSA. All participants underwent single night in-home or in-laboratory sleep testing with PSG (Nox A1, Resmed, Australia), with concomitant 3D scanning (Sense v2, 3D systems corporation, USA). Anthropometric data, comorbidities, medication, BERLIN, and NoSAS questionnaires were also collected at baseline. The PSG recordings were manually scored at the reference sleep center. The 3D craniofacial scans were processed by geometric morphometrics, and 13 different supervised algorithms, varying from simple to more advanced, were trained and tested. Results for OSAS recognition by ML models were then compared with
scores for specificity and sensitivity obtained using BERLIN and NoSAS questionnaires.
Results: All valid scans (n ¼ 267) were included in the analysis (patient mean age: 59 ± 9 years; BMI: 27 ± 4 kg/m2). For PSG-derived AHI15 events/h, the 56% specificity obtained for ML analysis of 3D craniofacial shapes was higher than for the questionnaires (Berlin: 50%; NoSAS: 40%). A sensitivity of 80% was obtained using ML analysis, compared to nearly 90% for NoSAS and 61% for the BERLIN questionnaire. The auROC score was further improved when 3D geometric morphometrics were combined with patient anthropometrics (auROC = 0.75).
Conclusion: The combination of 3D geometric morphometrics with ML is proposed as a rapid, efficient, and inexpensive screening tool for OSA.